Sex should be a fun, intimate experience, but for some women, it can sometimes feel painful instead. If you're experiencing discomfort during sex, you're not alone. In fact, pain during sex—known as dyspareunia—is a fairly common issue. There are several reasons why sex might hurt, and understanding a bit about female anatomy can help explain what’s going on.
Fun Medical Fact: Did you know that the clitoris has around 10,000 nerve endings, making it the most sensitive part of the human body? Just a little something to appreciate.
Understanding the Female Anatomy
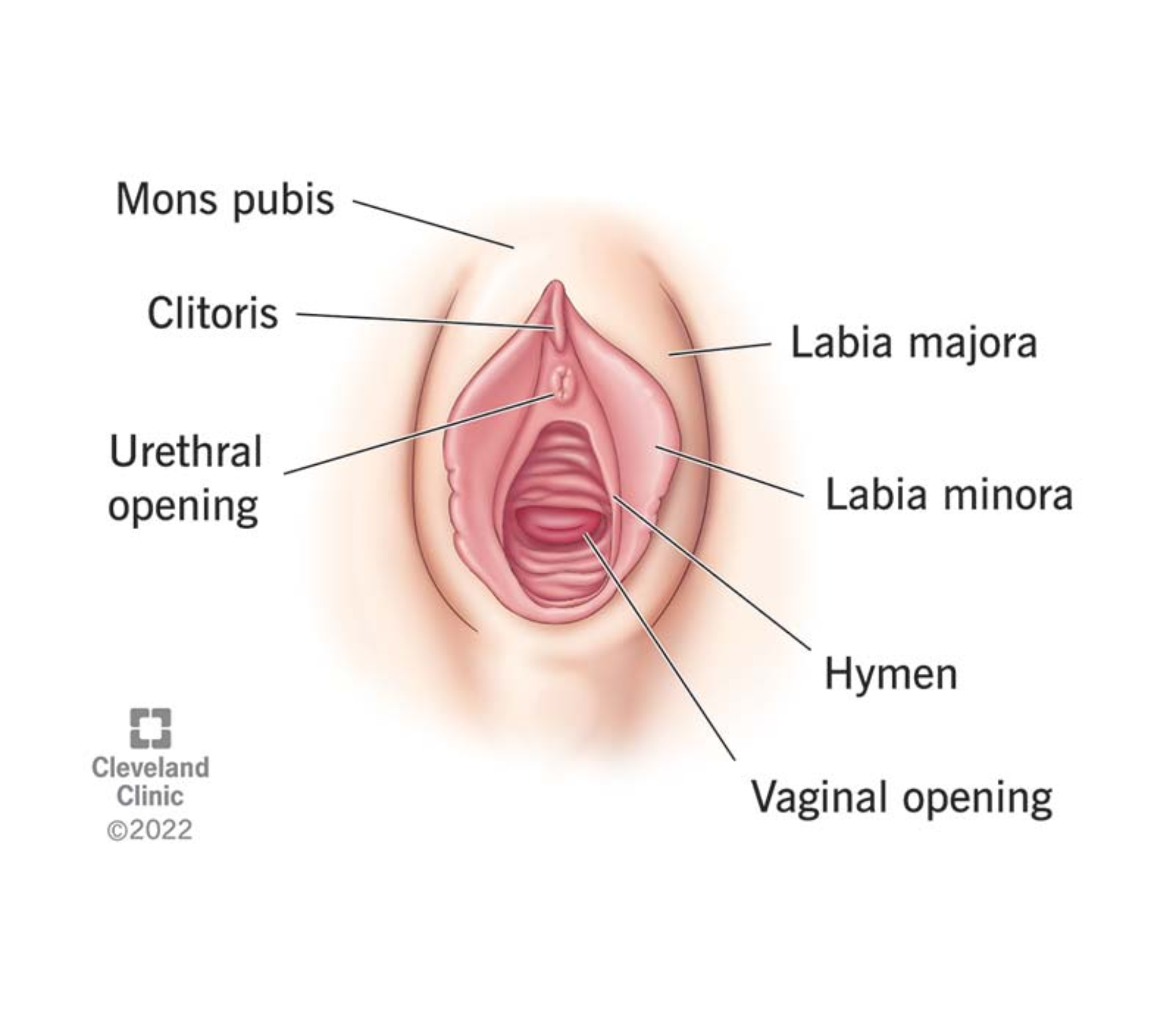
Let’s first take a quick dive into female anatomy, as it will help us understand why sex can sometimes cause discomfort:
- Vagina: The canal connecting the outside of the body to the cervix, where sperm is deposited during intercourse. It's designed to stretch and accommodate penetration.
- Labia: The external folds of skin surrounding the vaginal opening, which help protect the inner parts of the reproductive system.
- Cervix: The lower part of the uterus that connects to the vagina. It’s sensitive, and deep penetration can sometimes cause discomfort if it touches too forcefully.
- Pelvic Floor Muscles: A group of muscles supporting organs like the uterus and bladder. When tight or tense, these muscles can make penetration painful.
- Clitoris: Located above the vaginal opening, it's packed with nerve endings and plays a key role in sexual pleasure.
Now that we’ve gotten familiar with the anatomy, let’s take a look at why sex might hurt.
Common Reasons Why Sex Hurts
- Insufficient Lubrication
- One of the most common culprits of painful sex is insufficient lubrication. Your vagina naturally produces moisture, but sometimes, factors like hormonal changes, stress, or lack of foreplay can affect that. Without enough lubrication, sex can become uncomfortable or even painful. This is especially common during perimenopause or after childbirth when hormone levels fluctuate.
Fun Fact: A healthy vagina is naturally acidic, with a pH of about 3.8 to 4.5. This helps protect against infections, but it can also make dryness feel a bit worse.
2. Vaginismus
- Vaginismus occurs when the pelvic floor muscles involuntarily tighten during attempted penetration, making sex painful or even impossible. This condition can be caused by psychological factors like anxiety or past trauma, or physical factors like injury or infection.
Fun Fact: Vaginismus is often misunderstood and can be triggered by both psychological and physical factors. Interestingly, some people with vaginismus might not experience pain in other activities, like tampon insertion or pelvic exams, showing how unique this condition can be to sexual experiences.
3. Infections and Medical Conditions
- Infections such as yeast infections, UTIs, and STIs can lead to painful sex. These conditions cause inflammation, itching, and swelling in the vaginal area, making intercourse uncomfortable.
- Other chronic conditions, like endometriosis or pelvic inflammatory disease (PID), can also cause ongoing pain during sex.
Fun Fact: Did you know that the most common infection that causes painful sex is a
yeast infection? They’re caused by an overgrowth of a fungus that’s naturally present in the body. Although they’re super common, they’re also usually easy to treat with antifungal medications.
4. Pelvic Floor Dysfunction
- The pelvic floor muscles play a big role in sexual comfort. When they’re too tight or too weak, they can cause pain. Stress, trauma, or childbirth can lead to pelvic floor dysfunction, contributing to painful intercourse.
Fun Fact: The pelvic floor muscles are like a hammock that supports your bladder, uterus, and rectum. They can be compared to a suspension bridge—if any part of that "hammock" is too tight or too loose, it can affect everything it supports, including sexual comfort. Some people even do pelvic floor exercises (like Kegels) to help keep those muscles in tip-top shape.
5. Emotional or Psychological Factors
- Stress, anxiety, or past experiences can affect your ability to relax during sex, which can lead to pain. Sometimes, emotional factors like feeling disconnected from your partner or not feeling fully comfortable can physically manifest as discomfort during sex.
Fun Fact: The mind-body connection is powerful—did you know that sexual discomfort due to psychological factors can actually be helped by practicing mindfulness or relaxation techniques? The brain is such a powerful player in sexual experiences that focusing on relaxation can sometimes reduce physical pain.
6. Positioning and Communication
- Certain sexual positions can place extra pressure on the cervix or strain the pelvic muscles, leading to pain. Open communication with your partner about what feels good and what doesn’t is key to ensuring a more comfortable experience.
Fun Fact: Did you know that pillow support can make a big difference in comfort during intimate moments? Placing a pillow under the hips can help adjust angles, reduce pressure, and make positions feel more comfortable, giving you and your partner a better experience. It’s like a little "comfort boost" for the body.
When to Seek Help
If you’re experiencing pain during sex, don’t feel like you have to just “live with it.” There are
medical solutions available. It’s a good idea to talk to a healthcare provider if the pain is ongoing or severe. They can help identify the cause and offer treatment options.
Possible treatments include:
- Lubricants to ease dryness.
- Pelvic floor physical therapy to relax or strengthen muscles.
- Counseling or therapy to address emotional factors.
- Medication or surgery for conditions like endometriosis or infections.
Fun Fact: The body has the ability to self-lubricate, but it’s also really good at letting you know when something isn’t quite right. So trust your body, and don’t hesitate to ask for help if needed.
Pain during sex is common, but it doesn’t have to be your norm. Understanding your body, addressing any physical or emotional issues, and seeking help when necessary can lead to a more enjoyable and comfortable experience. Don’t hesitate to talk to your doctor—they’re there to help you improve your sexual health and overall well-being.
If you have more questions or need additional support, feel free to reach out to us at Almond so we can help guide you toward a healthier, more enjoyable sexual experience.



Don’t just get seen, get taken care of.
Questions? Call or book an Intro Call with a member of our team.
© 2024 All Rights Reserved
Almond
