
At Almond ObGyn, we know that your birth control needs are as unique as you are. Whether you're avoiding hormones for medical reasons or simply prefer a more natural approach, we offer a variety of non-hormonal and alternative birth control methods designed to fit your lifestyle. From copper IUDs to fertility awareness, let’s explore these highly effective, hormone-free options to help you stay in control of your reproductive health. Ready to find the method that’s right for you? Let’s dive in.
Non-Hormonal Birth Control Methods
1. Copper IUD (Intrauterine Device)
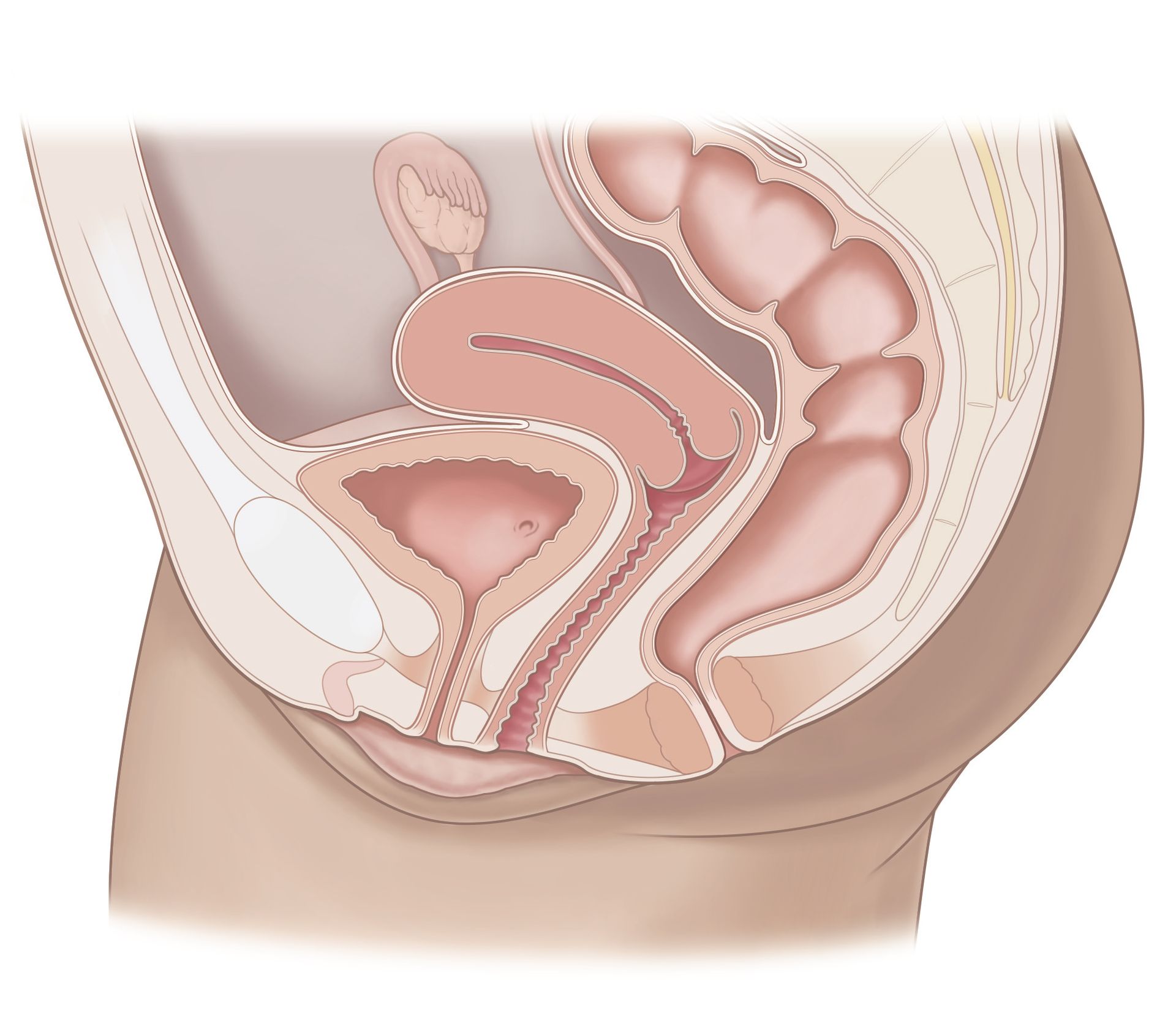
The copper IUD is one of the most reliable and hormone-free birth control options available. This small, T-shaped device is inserted into the uterus by a healthcare provider and works by releasing copper ions that create an environment hostile to sperm, preventing fertilization. It’s
over 99%
effective and provides long-lasting protection for up to
10 years.
Why It's Great
- No hormones involved—ideal for those who prefer a natural approach.
- Over 99% effective at preventing pregnancy.
- Once inserted, it’s hassle-free and offers long-term protection.
- It can stay in for up to 10 years but can also be removed earlier by a healthcare provider if desired.
What to Consider
- It may cause heavier periods or cramping in some users.
- Requires a healthcare provider for insertion and removal.
2. Barrier Methods
Barrier methods, like condoms, diaphragms, and cervical caps, create a physical barrier that blocks sperm from entering the uterus. They’re easy to use, available without a prescription, and completely hormone-free. Plus, many of these options help prevent sexually transmitted infections (STIs), too.
- Condoms: Not only do they prevent pregnancy, but they also protect against STIs. With perfect use, condoms are about
98%
effective. However, with typical use, they’re about
85%
effective.
- Diaphragms & Cervical Caps: These devices are inserted into the vagina before intercourse and cover the cervix to block sperm. Diaphragms are about 83% effective with typical use, and cervical caps range from 71% to 86% effective, depending on whether you’ve had children.
Why They’re Great
- No hormones—safe for those who want a natural method.
- Easy to access and use.
- Condoms offer the bonus of STI protection.
What to Consider
- Must be used consistently and correctly for the best results.
- Diaphragms and cervical caps require a prescription from your healthcare provider.
3. Fertility Awareness Methods (FAM)
Fertility Awareness Methods (FAM) are a collection of techniques that involve tracking your menstrual cycle and identifying the days when you’re most fertile. This method allows you to avoid unprotected sex during your fertile window to prevent pregnancy naturally—without the use of hormones. It is important to note that since
sperm can live for up to 5 days in the female reproductive system, precise tracking is essential for preventing pregnancy. If you miscalculate your fertile window and have unprotected sex just a few days before ovulation, sperm could survive long enough to fertilize the egg once it’s released.
How FAM Works
There are several ways to track your fertility using different signs and methods. The main techniques include:
- Basal Body Temperature (BBT) Charting: You track your body temperature first thing in the morning every day. Just before ovulation, your BBT will drop slightly, and then rise after ovulation, indicating that you’ve entered the fertile phase of your cycle. This method helps you pinpoint ovulation after it’s already occurred.
- Cervical Mucus Monitoring: You observe the consistency and appearance of your cervical mucus throughout your cycle. During your most fertile days (usually just before ovulation), cervical mucus becomes clear, stretchy, and similar to egg whites, indicating that you're in your fertile window.
- Calendar Method: This involves tracking the length of your menstrual cycles over several months and estimating your fertile window based on cycle patterns. This method is less reliable than other FAM techniques, as cycle length can vary from month to month.
- Ovulation Predictor Kits (OPKs): These test your urine for luteinizing hormone (LH), which spikes just before ovulation. While these kits help identify ovulation more precisely, they need to be used alongside other methods for full accuracy.
By combining one or more of these methods, FAM allows you to accurately identify when you're fertile and when to avoid unprotected sex. It requires a commitment to tracking your cycle consistently and being mindful of fertility signs.
Effectiveness of FAM
- Perfect Use: When done consistently and correctly, FAM can be up to
99%
effective. This means that fewer than 1–5 women out of 100 will become pregnant during the first year of perfect use.
- Typical Use: However, if the method is used with some inconsistencies or mistakes (e.g., miscalculating ovulation or not tracking signs consistently), the effectiveness drops to about 76%. This means 12 to 24 women out of 100 might become pregnant within the first year of typical use.
It’s important to note that the success of FAM depends heavily on
consistent and
accurate tracking of fertility signs like BBT, cervical mucus, and ovulation tests. Many users also pair FAM with barrier methods (like condoms) during their fertile window to increase effectiveness and reduce the risk of pregnancy.
Why It’s Great
- Completely natural and hormone-free, making it an ideal choice for those who want to avoid synthetic hormones.
- Cost-effective—there’s no need for ongoing prescriptions or doctor visits (except for initial guidance from a healthcare provider).
- Can be
combined with other methods (like condoms) for extra protection and peace of mind.
- Empowers you to learn more about your body and your cycle, increasing awareness of your reproductive health.
What to Consider
- Requires
consistent, accurate tracking of fertility signs (temperature, mucus, cycle dates, etc.).
- Less effective if not used perfectly. A single miscalculation can increase the risk of pregnancy.
- Doesn’t protect against STIs, so it’s a good idea to combine with barrier methods like condoms if STI protection is a priority.
Ideal Candidates for FAM:
FAM can be an excellent option for individuals who are highly motivated to learn about and track their fertility signs. It’s especially appealing to those who prefer a natural method or have medical conditions that make hormonal birth control options unsuitable. However, FAM requires diligence and commitment to tracking over time, so it might not be ideal for those who are looking for a “set it and forget it” method.
4. Sterilization
Sterilization is a permanent solution for birth control, perfect for those absolutely certain they do not want children in the future. It involves either tubal ligation (for women) or vasectomy (for men). This method is incredibly effective and doesn’t require ongoing maintenance.
- Tubal Ligation (for women): This procedure blocks or cuts the fallopian tubes, preventing eggs from reaching the uterus. It’s about
99.5%
effective.
- Vasectomy (for men): This procedure blocks or cuts the vas deferens, stopping sperm from mixing with semen. It’s 99.9% effective, but it’s important to note that it’s not immediately effective.
After a vasectomy, men must use another form of birth control until sperm are cleared from the semen, which can take around
3 months or
15 to 20 ejaculations. A healthcare provider will test sperm count to confirm the procedure was successful.
Why It’s Great
- Permanent, highly effective birth control.
- No need for ongoing maintenance or daily reminders.
What to Consider
- Permanent, so it’s a big decision.
- Requires surgery with a recovery period.
5. Withdrawal Method (Pull-Out Method)
The withdrawal method, or "pull-out" method, is when the male partner withdraws before ejaculation to prevent sperm from entering the vagina. Although it’s free and always available, it’s one of the least effective methods. With typical use, it’s about
78%
effective, meaning
22 out of 100 couples using this method will become pregnant each year.
Why It’s Great
- No cost and always available—no prescriptions required.
- No hormones involved.
What to Consider
- Requires precise timing and control, making it
less reliable.
- Does not protect against STIs.
Looking for Guidance Choosing the Right Birth Control?
At Almond ObGyn, we believe that choosing the right birth control method should be an empowering decision. Whether you're considering the copper IUD, exploring barrier methods, tracking fertility signs with FAM, or considering sterilization, our expert team is here to help you find the best option for your lifestyle. Ready to take the next step?
Book a visit today—we’re here to support you.
Disclaimer: Birth control effectiveness can vary based on individual factors. Always consult with your healthcare provider to choose the method best suited to your needs.


Don’t just get seen, get taken care of.
Questions? Call or book an Intro Call with a member of our team.
© 2024 All Rights Reserved
Almond
