
Polycystic Ovary Syndrome (PCOS) affects up to 13% of women of childbearing age, yet up to 70% of those affected remain undiagnosed worldwide. It's a leading cause of infertility and comes with a variety of symptoms that can be tricky to pin down and treat. But here's the exciting part: alongside traditional medical methods, there's growing evidence supporting an integrative approach through functional medicine for managing PCOS. That's where Almond steps in. We are dedicated to providing a comprehensive, personalized approach to PCOS care. Our goal isn't just to relieve symptoms but to get to the root causes, empowering women with effective strategies for both preventing and managing chronic health issues. Ready to take charge of your PCOS journey? Let's do this together.
Understanding PCOS through a Functional Lens
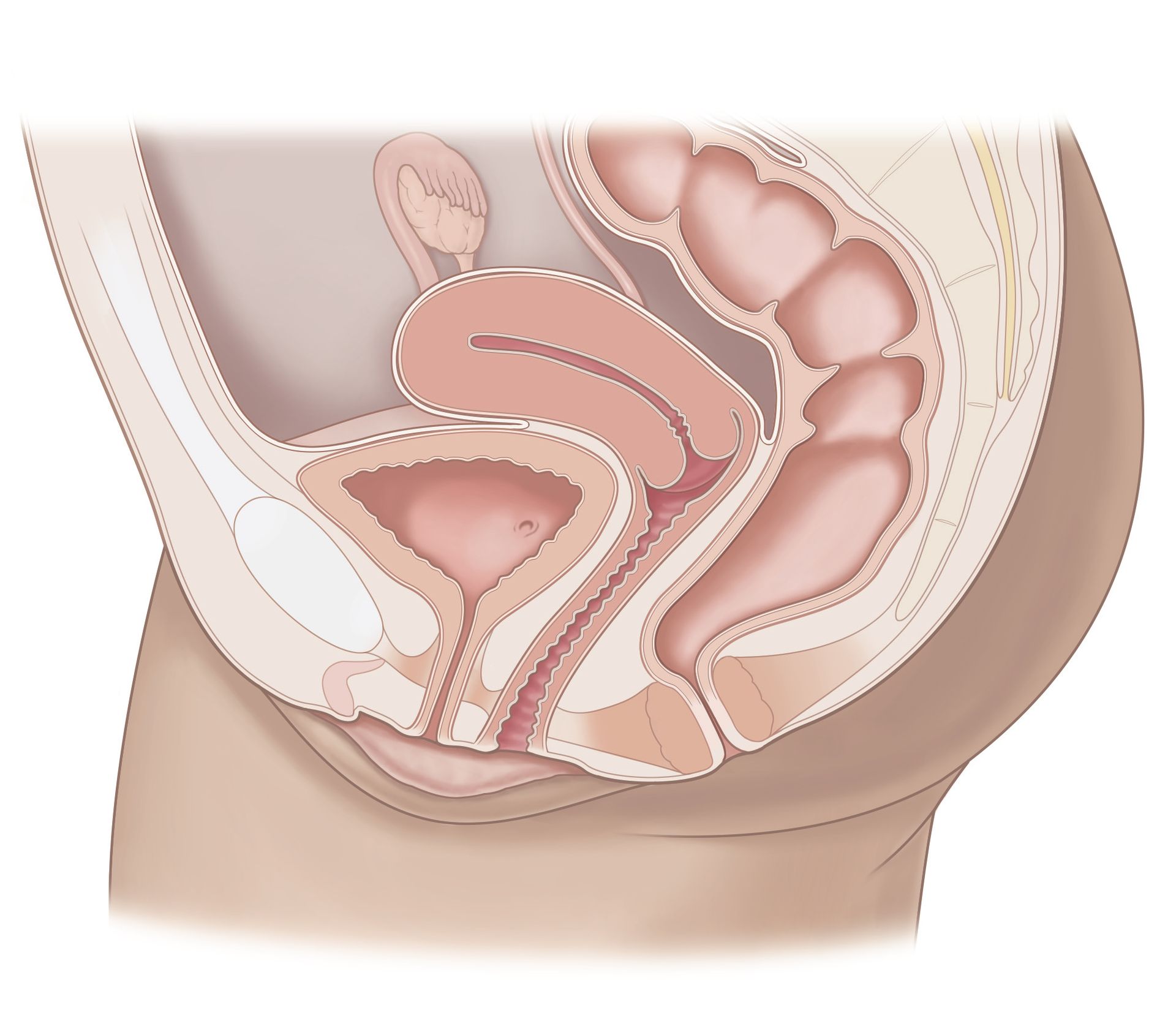
PCOS is characterized by hormonal imbalances, irregular menstrual cycles, ovarian cysts, and metabolic disturbances such as insulin resistance. It is termed a "syndrome" rather than a specific disease because it is characterized by a collection of symptoms that can vary in severity and presentation among individuals. Scientific understanding of PCOS is still evolving, and ongoing research is essential to clarify its underlying mechanisms and improve management strategies.
Conventional medicine often addresses PCOS symptoms with targeted medications, like hormonal birth control for menstrual irregularities or metformin for insulin resistance. While these medications can provide relief, they often serve as temporary fixes and do not address the underlying causes of PCOS. By focusing primarily on symptom management, they can overlook the underlying factors contributing to the condition. In contrast, a holistic functional medicine approach aims to uncover and address these root causes, offering a more comprehensive and effective solution.
Functional medicine sees PCOS as a complex condition shaped by genetics, environment, lifestyle, and nutrition. At Almond, we start by thoroughly assessing your medical history, lifestyle, and dietary habits to create a personalized healthcare plan tailored to your needs. Our approach goes beyond merely alleviating symptoms; we focus on restoring hormonal balance, improving metabolic function, and enhancing overall wellness. This comprehensive method not only addresses symptoms but also aims to achieve long-term health and lifestyle goals.
PCOS Insights: How a Functional Approach Can Transform Your Health
The Role of Nutrition and Lifestyle Modifications
Dietary interventions play a crucial role in the management of PCOS by influencing hormonal balance, insulin sensitivity, and overall metabolic health. Here's a look at some evidence-based data on how diet and lifestyle impacts PCOS:
In a study featured in the
American Journal of Clinical Nutrition, researchers found that women with PCOS who embraced a low-Glycemic Index (GI) diet for 12 weeks saw impressive boosts in insulin sensitivity. What does this mean? Well, low-GI diets help keep your blood sugar stable, which in turn reduces those pesky insulin spikes—a game-changer for managing PCOS, where insulin resistance often lurks.
Why is insulin relevant? Insulin spikes are problematic because they lead to insulin resistance, where cells become
less effective at using insulin, causing higher blood sugar levels and increased fat storage. For individuals with PCOS, frequent insulin spikes exacerbate insulin resistance, worsening hormonal imbalances and contributing to symptoms like weight gain, acne, and irregular periods. This cycle intensifies PCOS symptoms and complicates overall management of the condition.
Research featured in Human Reproduction Update, dug into the Mediterranean diet and its impact on PCOS. The findings reveal that adhering to this nutritious diet—rich in lean proteins, low in carbohydrates, and including beneficial fats from sources like olive oil and nuts—can have significant positive effects. It's been linked to better insulin sensitivity, less inflammation, and even more regular periods in women with PCOS. In this study, 86.7% of women on the mediterranean diet experienced a return to normal menstrual cycles. Seems like the Mediterranean diet isn't just about tasty meals—it's a powerhouse for balancing hormones and keeping your metabolism in top shape.
Moreover, lifestyle factors such as stress management, circadian rhythm, sleep patterns, and regular movement throughout the day are integral components of functional medicine interventions. A 2018 study published in Diabetes Care, explored how circadian rhythm disruption affects metabolic health in women with PCOS. It found that irregular sleep-wake cycles significantly impair insulin sensitivity and glucose metabolism. Specifically, women with circadian misalignment exhibited 20-30% greater insulin resistance compared to those with more consistent sleep patterns.
Lastly, stress hormones can exacerbate PCOS symptoms, and techniques such as mindfulness, yoga, or regular exercise can help mitigate their effects. Physical activity not only aids in weight management but also improves insulin sensitivity and promotes overall cardiovascular health, crucial for women with PCOS who are at higher risk of metabolic syndrome.
Comprehensive Testing
Navigating PCOS requires a well-rounded approach to testing that covers all aspects of health. This includes detailed hormonal assessments, metabolic profiling, and evaluations of nutritional status. By combining these elements, we gain a complete understanding of each individual's unique physiological needs. With these insights, Almond creates personalized treatments to rebalance hormones, improve metabolism, and enhance overall well-being. This method isn't just effective—it's tailored and evidence-based, aiming to achieve your best health from every angle.
Integrative Approaches and Evidence-Based Treatments
Here at Almond, we're big fans of integrative therapies like acupuncture, herbal supplements, and micronutrient therapies in managing PCOS. While the evidence varies, studies show they may help ease symptoms such as excess hair growth and irregular periods. In our functional medicine approach, we blend these therapies with conventional treatments to create a personalized plan that's just right for you.
Patient Empowerment
One of the greatest benefits of functional medicine for women with PCOS is its patient-centered approach, which Almond’s PCOS program is designed to deliver. Unlike traditional models where doctors provide brief instructions and expect perfect adherence, our program focuses on ongoing conversations and collaboration. At Almond, we prioritize listening to patients' insights about their own bodies, offering comprehensive education on their conditions and treatment plans, and adjusting treatments based on real results and patient feedback. By empowering patients to make informed changes and supporting them through lifestyle adjustments, functional medicine helps achieve better health outcomes.


Don’t just get seen, get taken care of.
Questions? Call or book an Intro Call with a member of our team.
© 2024 All Rights Reserved
Almond
