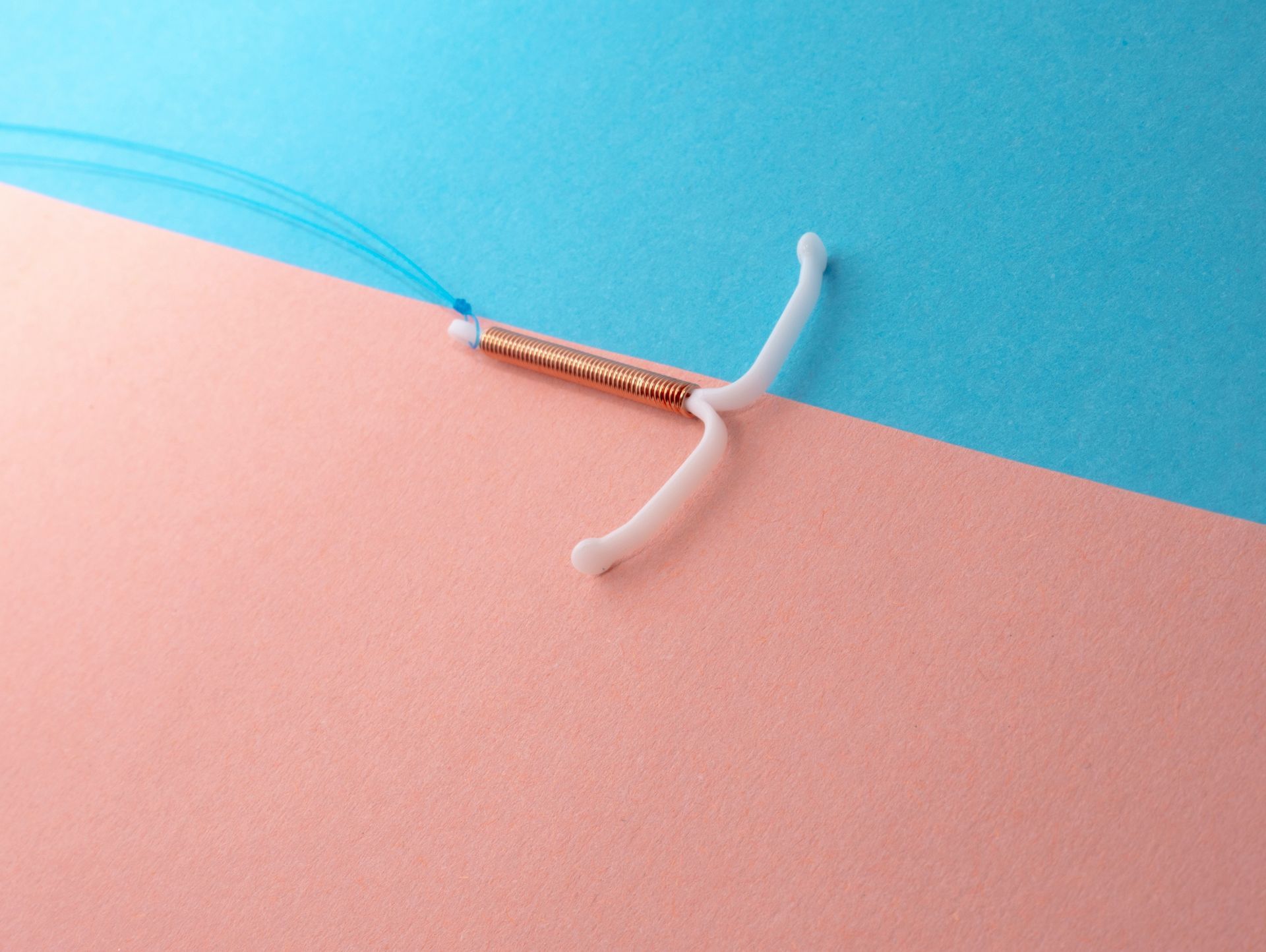
In recent discussions spurred by the new CDC guidance on IUD insertion, the discomfort associated with IUD (intrauterine device) insertion has gained increased attention. It’s a procedure that many find daunting, but understanding how we work at Almond to minimize pain can help ease some of those anxieties.
At the heart of our approach to IUD insertion is a commitment to patient comfort and care. We recognize that any medical procedure can be stressful, but there are several well-evidenced strategies we use to make the experience as smooth and pain-free as possible.
Preparation is Key
A portion of discomfort during IUD insertion comes from the unknown. To help you prepare, we make sure to provide you with all the important information you need in advance.This detailed guide helps patients mentally and physically prepare for the procedure. Knowing what to expect can significantly reduce anxiety and make the process feel less intimidating.
Pain Management Strategies
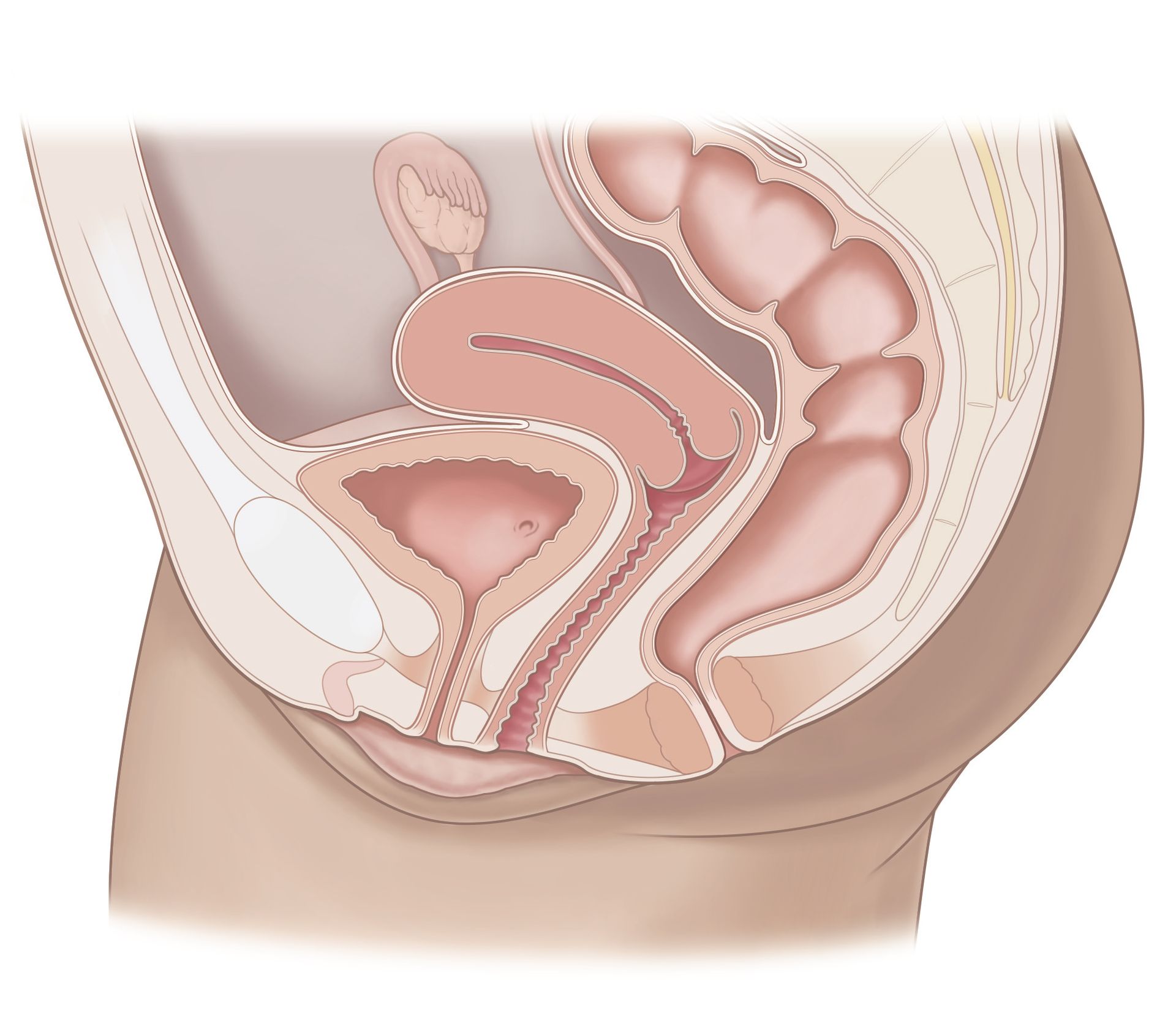
- Optimal Timing: If possible, scheduling the insertion during your menstrual period can be beneficial. During menstruation, the cervix is naturally slightly open, which can make the insertion process smoother and less uncomfortable.
- Pre-Procedure Pain Relief: We recommend that patients take 600 mg of ibuprofen about an hour before their scheduled appointment, unless there are medical contraindications. Ibuprofen helps to minimize cramping and discomfort.
- During the Procedure: To ensure patients are as comfortable as possible, we provide a detailed walkthrough of the procedure. We keep our patients informed about each step to prevent any surprises. To help with cramping, we use a heating pad on the lower abdomen and apply topical lidocaine to numb the cervix, reducing the pain associated with the insertion instrument.
Tailoring Comfort to Individual Needs
We understand that every patient is different, and comfort levels can vary widely. Therefore, we offer several additional options for managing discomfort:
- Anxiety Management: For patients who are particularly nervous, we offer anxiety-reducing medications. These can help ease emotional stress and make the procedure more manageable.
- Paracervical Block: Although not universally preferred due to potential discomfort, a paracervical block is available for those who may need it. This local anesthetic is administered via an injection around the cervix to reduce pain, but its effectiveness and comfort can vary.
- Sedation Options: For patients who require it, we can perform the IUD insertion under sedation in the operating room. This option is particularly useful for those with severe anxiety or who have experienced significant discomfort in previous procedures.
While the idea of IUD insertion may initially seem a bit overwhelming, here at Almond we are dedicated to making the experience as comfortable as possible. With careful preparation, thoughtful pain management, and personalized care, we strive to make your IUD insertion as smooth as it can be. We understand that this can be a sensitive topic, so if you have any concerns or questions about the procedure, please feel free to reach out to us at any time. We are here to support you and guide you through every step of the process with empathy and care.
Book care with Almond
here.


Don’t just get seen, get taken care of.
Questions? Call or book an Intro Call with a member of our team.
© 2024 All Rights Reserved
Almond
