The percentage of U.S. women in the workforce and the number of hours we work have steadily increased over the last several generations. But what about the amount of work involved in pregnancy? That has largely stayed the same — or, arguably, increased.
Pregnancy risks have risen over time: women are having children later in life, maternal mortality rates have increased, and there is a growing need to protect against higher levels of toxins in our environment and the stressors we face in daily life.
It’s time for our model of pregnancy care to change. The standard that worked for our mothers is no longer enough for us.
What is the standard pregnancy care model today?
To begin, we need to understand what the traditional model looks like and where it falls short. In a typical ObGyn practice that accepts your insurance, the standard of care today involves about 15 individual appointments. The longest visit often lasts around 20 minutes, and many appointments are as short as 5 minutes. Many women report feeling anxious, uncertain, or afraid during their pregnancies. Between visits, they are often left with unanswered questions or overwhelming anxiety.
It doesn’t have to be this way. As we set out to build better ObGyn care at Almond, we asked ourselves: What’s working well today, and how can we make it even better?
We discovered a model that works significantly better than traditional pregnancy care: group pregnancy care.
What is group pregnancy care?
This model involves around ten 90-minute sessions led by a midwife, along with 4-5 individual appointments with an ObGyn. The longer sessions provide more thorough education on pregnancy, giving each woman the information she needs to make informed decisions, rather than relying on brief, intermittent medical visits.
Even more importantly, the group format fosters community—something that is essential in a country where loneliness has become so widespread that the Surgeon General has classified it as an epidemic. Pregnancy is no exception. Historically, women have been socialized to experience pregnancy within a supportive community, and research has repeatedly shown that this group format is linked to better outcomes for both mother and baby.
This is one of the things we love about group pregnancy care — we didn’t invent it at Almond. The program, officially named Centering Pregnancy, was developed by Sharon Schindler Rising, a Yale-trained midwife and professor, and has been extensively studied and tested over the past couple of decades.
How does group care impact outcomes?
The better outcomes of this model speak for themselves. Studies have shown that group care reduces NICU admissions over 30% across various populations. A South Carolina Retrospective Cohort Study found that participation in group care reduced the risk of premature birth by 36%, resulting in an average cost savings of $22,667. The study also found that group care reduced the rate of low birthweight by 44%, saving an average of $29,627 per birth, and reduced the risk of a NICU stay 28%, with average savings of $27,249.
March of Dimes also reported that of group care helped patients “decrease c-sections from 28% to 21%, preterm births from 8.3% to 1.8% and decreased low birthweight from 8.3% to 2.65%.” Additionally, a pilot program run by BlueChoice Health Plan South Carolina resulted in a 3.5% NICU admission rate compared to a 12.0% to those receiving individual care. A retrospective study found that 83% (24 of 29) of studies found that low social support increases postpartum depressive symptoms.
How do Midwives impact care quality?
There is another significant impact to consider as well – how midwives impact prenatal care. The Cesarean birth rate is shown to be 12% lower when midwives are on the birth team. Midwives have shown to improve outcomes by 56 different measures—including lower morbidity and mortality among mothers and newborns, fewer preterm births and low birthweight infants, and reduced interventions during labor.
A recent analysis found that a midwife workforce, integrated into health care delivery systems, could provide 80 percent of essential maternal care globally. This approach has the potential to avert 41% of maternal deaths, 39% of neonatal deaths, and 26% of stillbirths globally.
How do modern care models impact Black women?
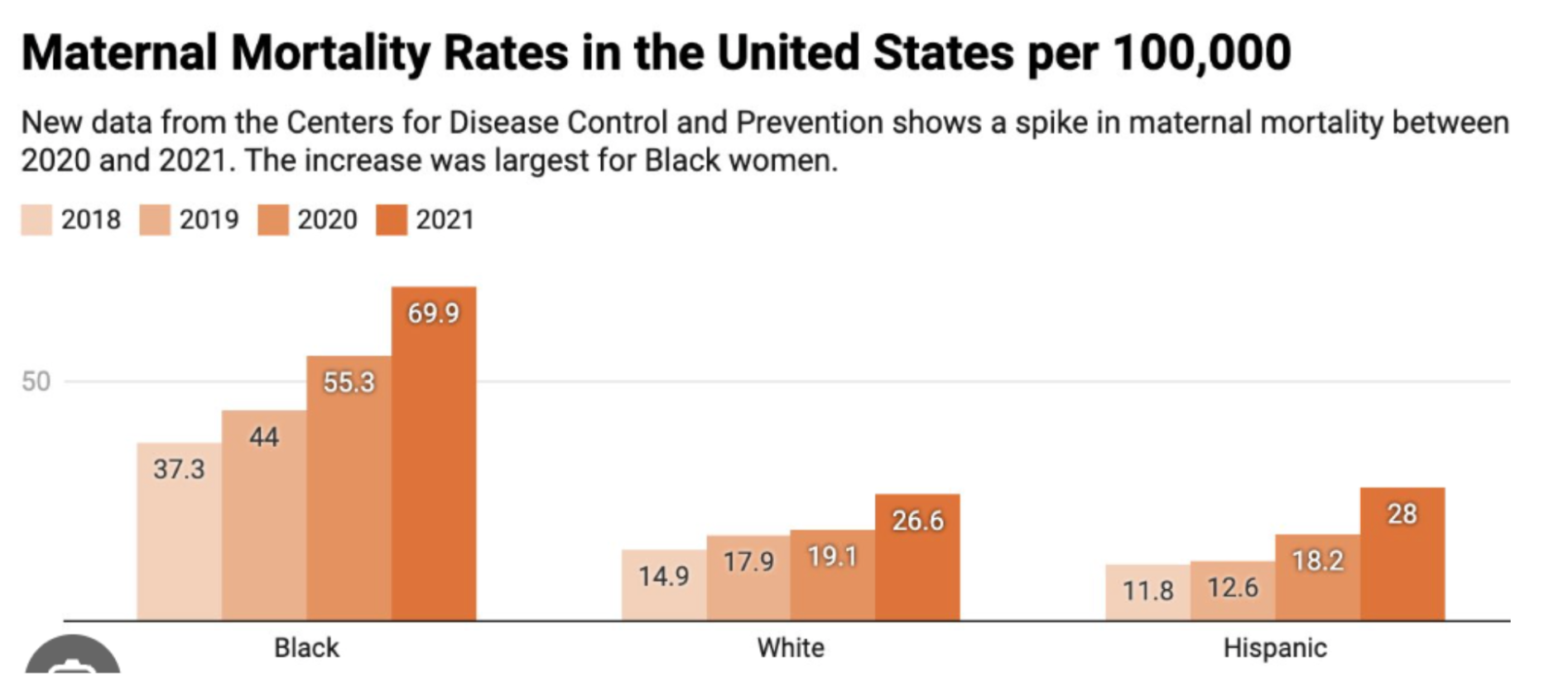
The impact is especially promising for Black women, who have long faced health discrimination and continue to experience worse outcomes. In the U.S., Black women experience a postpartum death rate that is 2.6 times higher than that of white women.
Source: Margo Snipe
Worse, the rate of Black maternal mortality is increasing; it surged by 26% in 2021. As the New York Times reported, “The richest Black women have infant mortality rates at about the same level as the poorest white women. The babies born to the richest Black women (the top tenth of earners) tended to have more risk factors, including being born premature or underweight.”
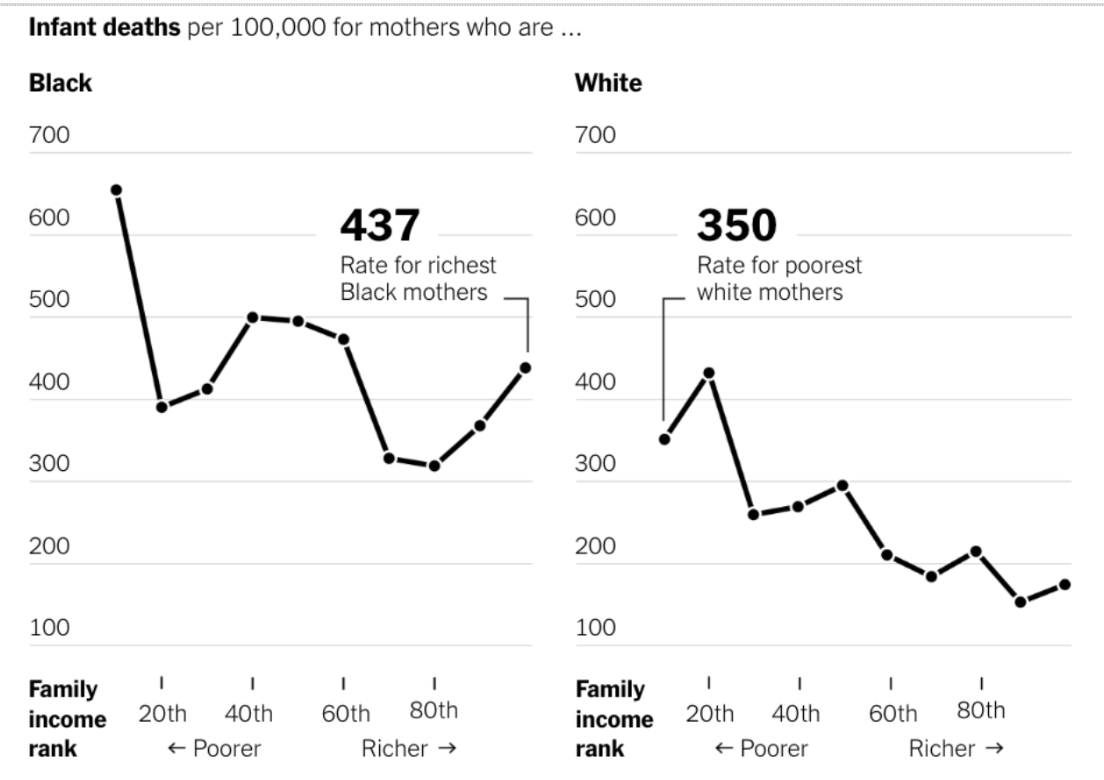
Source: New York Times
This is another reason we believe in the power of group care. The improved outcomes for low birth weight and pre-term birth offer hope, particularly for Black women.
Where can I get group pregnancy care?
The good news? Group pregnancy care is available in the majority of states across the country. You can
find locations in your state here.
Building on this foundation, at Almond we believe the next step is to enhance this great work by integrating technology to collect more and better data. This allows our provider team to have a clearer picture of each patient’s health, enabling us to deliver true preventative healthcare and identify and address potential issues sooner. That’s why we collect vital metrics such as blood pressure, weight, and blood sugar – and we collect them sooner and more regularly than a traditional ObGyn.
By combining the best of group care with modern data collection, at Almond, we’re not just changing the way we deliver pregnancy care—we’re improving outcomes and empowering women to make informed decisions about their health.
As a result, Almond is uniquely positioned to redefine the pregnancy care experience. Our approach is not just about reducing the risks of complications but about offering a truly supportive, informed, and connected journey through pregnancy—ultimately helping to create healthier futures for both mothers and babies. Whether you’re looking for group care in Los Angeles or learning about new, evidence-backed ways to support your pregnancy, Almond is here to change the trajectory of maternal care, one woman at a time.


Don’t just get seen, get taken care of.
Questions? Call or book an Intro Call with a member of our team.
© 2024 All Rights Reserved
Almond